How Much Promethazine To Get High
Promethazine, initially developed in France in the 1940s, was approved for use in the U.S. in 1951. The drug is not only used in the treatment of allergic reactions, such as hay fever, but it can also be used as a sedative, to prevent motion sickness, and to treat nausea and vomiting (including morning sickness).
A year after it entered the U.S. market, a combination drug of promethazine hydrochloride and codeine (a prescription narcotic) was introduced for common-cold symptoms and cough. However, the substance has also been misused as a potentially dangerous illegal street drug called "drank" or "sizzurp."

Promethazine can be administered orally as a tablet, through the rectum as a suppository and intravenously by injection
Promethazine can be administered orally as a tablet or in liquid form, through the rectum as a suppository, and intravenously by injection. If promethazine is given intravenously without proper caution, it is possible for the drug to move out of the blood vessels and into the surrounding tissue (a process called extravasation). This may cause potentially irreversible damage to tissues such as the skin, including gangrene (a dangerous, potentially fatal condition that involves the loss of blood flow to an area of tissue, causing it to break down and die). Instead, promethazine should be given by intramuscular injection.
This risk for extravasation prompted a boxed warning (the most serious drug labeling warning) from the U.S. Food and Drug Administration in late 2009. This was the second boxed warning for promethazine, with the first being required in 2006 after the FDA received reports of fatal respiratory depression (inadequate ventilation or increased concentrations of carbon dioxide) in children.
These severe, potentially life-threatening side effects are rare. More common and less severe side effects of promethazine commonly include drowsiness, dizziness, and dry mouth.
What Does Promethazine Treat?
Promethazine can relieve symptoms of allergic reactions when used as an antihistamine.
Promethazine helps relieve the symptoms of allergic reactions such as:
- Allergic rhinitis (runny nose and watery eyes)
- Allergic conjunctivitis (red, watery eyes)
- Allergic skin reactions (rash, hives)
- Allergic reactions to blood or plasma products
It can also be used in combination with other medications, such as epinephrine, to treat anaphylaxis (a sudden, severe allergic reaction) once the condition is controlled, as well as in combination with codeine for symptoms of the common cold, such as cough.
Although primarily used to treat allergies, promethazine is indicated to treat a variety of other conditions as well.
Promethazine can also be used for the following conditions:
- Sedation, to calm and to produce a light sleep in patients, before and after surgery, during labor and at other times
- To prevent and to treat motion sickness
- To prevent and to control nausea and vomiting associated with certain types of anesthesia and post-surgery
- In combination with analgesics (painkillers) to help control pain after surgery
- Intravenously in special surgical situations
How Does Promethazine Work?
Promethazine is used as a histamine-receptor blocker. Histamine receptors are proteins that bind with histamine to produce allergic reactions. This makes promethazine an effective antihistamine. The drug also blocks acetylcholine receptors, making it useful to prevent and treat nausea, morning sickness and cough. Promethazine can only help control symptoms. It isn't effective in treating the cause of symptoms or in speeding recovery, according to the National Institutes of Health (NIH).
Promethazine Side Effects
Promethazine can cause many different side effects, some common and some serious. These side effects can affect several different body systems and organs including the brain, heart, skin, blood, stomach and intestines and lungs.
The two most serious side effects of promethazine are addressed in a boxed warning on the drug's labeling. These reactions include respiratory depression, which can be fatal (occurring primarily in children under the age of 2 years) and, when promethazine is given intravenously, severe chemical irritation and tissue damage, including gangrene.
Common promethazine side effects:
- Drowsiness
- Difficulty falling asleep or staying asleep
- Dry mouth
- Nightmares
- Dizziness
- Blurred or double vision
- Vomiting
Serious promethazine side effects:
- Slowed breathing
- Fast or irregular pulse or heartbeat
- Abnormal or uncontrollable movements
- Hallucinations (seeing things or hearing voices that do not exist)
- Confusion
- Overwhelming or unmanageable fear or emotion
- Seizures
- Unusual bruising or bleeding
- Uncontrolled eye movements
Promethazine's Black Box Warnings
Promethazine hydrochloride-containing products administered by injection contain two boxed warnings. A boxed warning is the most serious type of warning issued by the FDA for drugs and medical devices, meaning that the side effects can cause serious injury and possibly death.
The first boxed warning for promethazine was added in late 2004. Serious and sometimes fatal adverse events, including respiratory depression, oversedation, agitation, hallucinations, seizures, and dystonic reactions or movement disorders, have been reported in children, according to the New England Journal of Medicine (NEJM).
Black box warning label for the promethazine drug Phenergan
In 1995, the American Academy of Pediatrics took steps to discourage the use of promethazine as an anesthetic premedication in children when used with other drugs that may cause respiratory depression.
In 2000, the warnings section of the label was strengthened to recommend that promethazine not be used in children younger than 2 years of age, and that it be used with caution in older children.
However, the FDA continued to receive adverse event reports, including fatal respiratory depression in young children, most of whom were under 2 years of age. Serious outcomes, including death, disability, life-threatening events, and hospitalization, occurred with all routes of administration, whether oral, rectal or intravenous injection.
"The unpredictable nature of adverse events and their serious outcomes justified further strengthening of warnings and contraindications and the addition of a boxed warning for the use of promethazine in children."
The boxed warning now clearly reads that promethazine hydrochloride injections should not be used in pediatric patients less than 2 years of age because of the potential for fatal respiratory depression. It also advises caution should be exercised when administering the drug in the form of an injection to patients 2 years and older.
In 2006, an FDA alert advised all health care professionals that the warning extended to promethazine hydrochloride (including brand name Phenergan and generic versions of the drug) in any form, whether syrups, suppositories, tablets or injectables.
Promethazine's Risk of Tissue Injury
In 2009, the FDA required a second boxed warning for promethazine hydrochloride injection to warn patients of the risks of severe tissue injury with injectable administration, including gangrene and necrosis (death of a body tissue when there is not enough blood flow to the tissue).
Did You Know
The FDA advised manufacturers to include in the boxed warning that the preferred route of administration for injectable promethazine is directly into a muscle.
Because of the risk for tissue injury with administering injectable promethazine both intravenously and subcutaneously (into the layer of skin directly below the dermis and epidermis), the FDA advised manufacturers to include in the boxed warning that the preferred route of administration for injectable promethazine is deep intramuscular injection (directly into a muscle).
Promethazine should not be given by intra-arterial injection (within an artery) under any circumstances because it may cause severe arteriospasm (spasm in an artery) and result in gangrene. In fact, the Institute for Safe Medication Practices now recommends that injectable promethazine should be eliminated from hospital use.
Purple Drank SIzzurp
The misuse of a liquid syrup combination of promethazine hydrochloride and codeine (an opioid pain reliever), indicated to treat common cold symptoms and cough, has become "increasingly popular among youth in several areas of the country," according to the National Institute on Drug Abuse. The syrup may be mixed with alcohol or flavored sodas and consumed for its mind-altering or mood-boosting effects, and may be referred to as "purple drank" or "sizzurp".
The prescription cough syrup has been known to sell on the streets for upwards of $1,000, with one brand (that the company stopped distributing in 2014) selling for as much as $3,000, Bloomberg said in 2017.

The prescription cough syrup is also known as "purple drank"
"It's the caviar of drugs," said Ronald Peters, a retired professor of behavioral sciences at the University of Texas Health Science Center in Houston.
It was reported that promethazine codeine syrup was prescribed about 4 million times in the U.S. in 2016, bringing in about $15 million in sales.
The U.S. Department of Health and Human Services reported that 11,000 emergency room visits occurred in the United States in 2011 (the most recent year for which data is available) as the result of codeine misuse. The boxed warning in the label of promethazine/codeine syrup now includes a warning regarding the risk for abuse, misuse, and addiction.
How Is Promethazine Administered?
Promethazine can be administered by mouth in solid (tablet) or liquid (solution or syrup) form, by injection (intravenously or intramuscularly), or into the rectum in the form of a suppository. When taking liquid promethazine, patients should use a measuring spoon or cup made specifically for measuring medications, and not a household spoon. The suppository can only be inserted through the rectum (lower part of the large intestine through the anus), and should not be swallowed.
Prior to removing the wrapper, if a suppository feels soft, the patient should first hold it under cold, running water for one minute. After removing the wrapper, the tip of the suppository should be dipped in water prior to insertion, using the finger. In adults, the suppository should be inserted into the rectum by one inch and by about one-half to one inch in children 2 and older.
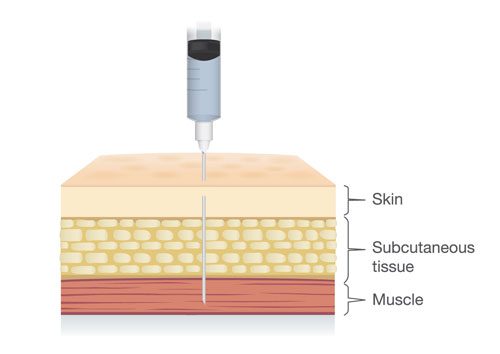
Deep intramuscular injection is the preferred method of promethazine injection
Since promethazine administered intravenously can cause severe chemical irritation and damage to tissues, deep intramuscular injection is the preferred method of injection.
Subcutaneous injection is also not advised because it may result in chemical irritation and damage to tissues, including necrosis.
Promethazine Dosages
Dosing for patients taking promethazine may vary based on the condition being treated, a patient's age and weight, other medications that a patient may be taking and other medical conditions that they may have.
Dosages by Condition:
- Allergic Conditions
- The average adult dose is 25 milligrams of promethazine. The dose may be increased or decreased or given several times daily, based on symptoms.
- Sedation
- In hospitalized adults, 25 to 50 milligrams of promethazine injection is recommended to achieve sedation.
- Nausea and Vomiting
- The usual adult dose of promethazine for nausea and vomiting is 25 milligrams. When adult patients cannot swallow tablets for nausea and vomiting, promethazine suppositories may be given at a dose of 12.5 to 25 milligrams. Doses may be given every four to six hours. The usual dose of promethazine for children with nausea and vomiting is 0.5 milligrams per pound of body weight, which may be adjusted based on age, weight, and symptoms.
- Before and After Surgery
- In adults, the usual dose of promethazine is 50 milligrams prior to undergoing surgical or obstetric procedures. In children, the usual dose is 0.5 milligrams per pound of body weight.
- Pediatric Patients
- Promethazine should not be used in children less than 2 years of age, and it should be used with caution in children older than 2 years. When given to children older than 2 years of age, the lowest effective dose should be used.
- When Administered Intravenously
- Promethazine can potentially interact with a number of other medications. Taking promethazine with certain medications can decrease the effectiveness of either drug or increase a patient's risk of unwanted side effects.
Promethazine & Drug Interactions
Promethazine can potentially interact with a number of other medications. Taking promethazine with certain medications can decrease the effectiveness of either drug or increase a patient's risk of unwanted side effects.
Medicines and other substances that may interact with promethazine include:
- Alcohol
- Acetycholinesterase inhibitor medications – used to treat dementia in patients with Alzheimer's disease
- Anticholinergic drugs – used to treat a variety of conditions including dizziness, gastrointestinal disorders, insomnia (short-term), respiratory disorders and sinus bradycardia (a heart beat that is regular but slower than normal)
- CYP 2B6 inhibitor medications, such as Paxil (paroxetine) and Zoloft (sertraline). The effects of these drugs may be increased when taken together with promethazine.
- CYP 2D6 inhibitor medications, such as Chlorpromazine, Prozac (fluoxetine), miconazole, Paxil (paroxetine), quinidine and Norvir (ritonavir). The effects of these drugs may be increased when taken together with promethazine.
- Epinephrine (adrenaline) – a hormone, neurotransmitter (messenger in the brain) and medication
- Monoamine Oxidase Inhibitors (MAOIs) – used for the treatment of depression
- Pramlintide (Symlin) – used to treat diabetes by lowering blood sugar levels
Other medications that can cause drowsiness, such as:
- Antipsychotic medications
- Anxiety medications
- Most antidepressants
- Muscle relaxants
- Narcotic pain relievers
- Sleep medications
- Some antihistamines
How Much Promethazine To Get High
Source: https://www.drugwatch.com/promethazine/
Posted by: rodriguezplad1987.blogspot.com

0 Response to "How Much Promethazine To Get High"
Post a Comment